As I reflect on my years as an emergency room doctor, I’m reminded of the countless times I’ve seen patients struggle with the neuroscience of depression. It’s a condition that’s often shrouded in mystery, with many people believing it’s just a matter of “snapping out” of it or that it’s a sign of weakness. But I’ve seen firsthand the _devastating impact_ it can have on individuals and their loved ones. The truth is, depression is a complex condition that requires a comprehensive understanding of the brain’s intricate workings.
In this article, I promise to cut through the noise and provide you with evidence-based insights into the neuroscience of depression. I’ll share my personal experiences, _backed by scientific research_, to help you understand the underlying mechanisms of this condition. My goal is to empower you with knowledge, not to perpetuate myths or hype. I’ll guide you through the latest findings and _practical applications_, so you can make informed decisions about your mental health. By the end of this journey, you’ll have a deeper understanding of the neuroscience of depression and how to navigate it with confidence.
Table of Contents
Unpacking Neuroscience of Depression

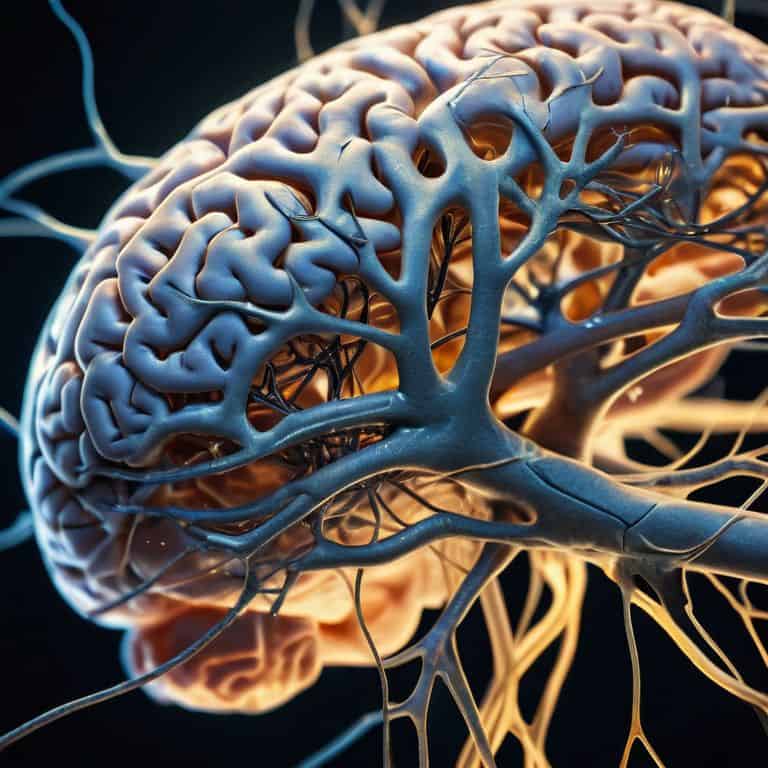
As I delve into the complexities of depression, I’m reminded of the neuroplasticity that underlies our brain’s ability to adapt and change. This concept is crucial in understanding how depression can rewire our brain’s functioning, often leading to a vicious cycle of negative thoughts and emotions. Research has shown that individuals with depression exhibit altered neural connections, which can be influenced by factors such as stress hormones and gut health.
The interplay between our gut and brain is a fascinating area of study, with emerging evidence suggesting that depression and gut health are intimately linked. The gut microbiome produces neurotransmitters that regulate mood, and an imbalance of these chemicals can contribute to depressive symptoms. Furthermore, the brain-derived neurotrophic factor (BDNF) plays a critical role in neuroplasticity, with decreased levels often associated with depression.
In my experience as a doctor, I’ve seen how neurotransmitter imbalance symptoms can manifest differently in each patient. While some may exhibit classic symptoms of depression, others may present with anxiety, insomnia, or irritability. Effective treatment of major depressive disorder requires a comprehensive approach, taking into account the complex interplay between genetic, environmental, and lifestyle factors. By acknowledging the intricate relationships between these factors, we can work towards developing more personalized and effective treatment options.
Neuroplasticity and Gut Health Linked
As I delve into the complexities of depression, I’m reminded of the interconnectedness of our brain and body. Recent studies have shed light on the intricate relationship between neuroplasticity and gut health, revealing a profound impact on our mental well-being.
The gut-brain axis plays a crucial role in this dynamic, with microbiome balance influencing the production of neurotransmitters that regulate mood and cognition.
Stress Hormones Impact Mental Health
As I delve into the complexities of depression, I’m reminded of the crucial role stress hormones play in mental health. These chemicals, such as cortisol, can have a profound impact on our well-being, influencing everything from mood to motivation. When stress hormones are elevated, it can be like a constant alarm blaring in the background, making it difficult to focus or find peace.
In my experience as a doctor, I’ve seen how chronic stress can lead to hormonal imbalances, which in turn can exacerbate symptoms of depression. By understanding the interplay between stress hormones and mental health, we can begin to develop more effective strategies for managing stress and promoting resilience.
Beyond the Dark Cloud of Depression

As I delve deeper into the complexities of depression, I’m reminded of the neuroplasticity and depression connection. It’s fascinating to see how our brain’s ability to adapt and change can be both a blessing and a curse. On one hand, neuroplasticity allows us to rewire our thoughts and behaviors, offering a glimmer of hope for recovery. On the other hand, it can also perpetuate negative patterns, making it challenging to break free from the cycle of depression.
My experience as a doctor has taught me that depression and gut health are intimately linked. The gut-brain axis plays a crucial role in regulating our mood, and an imbalance of gut bacteria can exacerbate depressive symptoms. By addressing gut health through dietary changes and probiotics, patients can experience a significant improvement in their mental well-being. It’s essential to recognize that depression is not just a mental health issue, but also a physical one, and stress hormones and mental health are intricately connected.
As we explore the intricacies of depression, it’s clear that a neurotransmitter imbalance can have far-reaching consequences. The interplay between neurotransmitters like serotonin and dopamine can either contribute to or alleviate depressive symptoms. By understanding the complex relationships between these chemicals, we can develop more effective treatment strategies, including therapies that target brain derived neurotrophic factor and depression. This knowledge can help us move beyond the dark cloud of depression, offering a beacon of hope for those struggling with this condition.
Bdnf and Treatment Options Revealed
As I delve into the complexities of depression, I’m reminded of the crucial role brain-derived neurotrophic factor (BDNF) plays in our mental well-being. This protein is essential for the growth and maintenance of healthy neurons, and its dysregulation has been linked to various neurological disorders, including depression.
In my experience as a doctor, I’ve seen how targeted therapies can help increase BDNF levels, leading to improved symptoms in patients. By focusing on evidence-based treatments, such as exercise and cognitive-behavioral therapy, we can work towards unlocking the full potential of BDNF in combating depression.
Neurotransmitter Imbalance Symptoms Explored
As I delve into the complexities of depression, I’ve come to realize that neurotransmitter imbalance plays a significant role in its development. This imbalance can manifest in various ways, affecting mood, appetite, and sleep patterns. I’ve seen patients struggle with feelings of hopelessness and worthlessness, often accompanied by physical symptoms like fatigue and changes in appetite.
The symptoms of neurotransmitter imbalance can be subtle, but persistent feelings of sadness can be a telling sign. As a doctor, I’ve learned to look beyond the surface-level symptoms and explore the underlying biological mechanisms that contribute to depression. By understanding these complexities, we can work towards developing more effective treatment plans that address the root causes of this debilitating condition.
5 Evidence-Based Strategies to Understand and Manage Depression
- Practice Mindfulness to Enhance Neuroplasticity: Regular mindfulness exercises can help rewire the brain, promoting positive changes in neural connections and potentially alleviating depressive symptoms
- Maintain a Balanced Gut Microbiome: A healthy gut-brain axis is crucial; focus on consuming fermented foods, omega-3 rich foods, and consider probiotics to support gut health
- Monitor and Manage Stress Hormones: Engage in stress-reducing activities like yoga, meditation, or long-distance cycling to keep cortisol levels in check and support mental well-being
- Focus on Sleep Hygiene for Neurotransmitter Regulation: Prioritize a consistent sleep schedule, avoid caffeine and electronics before bedtime, and create a sleep-conducive environment to help regulate neurotransmitters
- Explore BDNF-Boosting Activities for Improved Mental Health: Engage in activities that promote the production of brain-derived neurotrophic factor (BDNF), such as reading, learning a new skill, or enjoying a cup of gourmet coffee while practicing a hobby, to support neuronal health and resilience
Key Takeaways on the Neuroscience of Depression
I’ve found that understanding the interplay between neuroplasticity, gut health, and stress hormones is crucial in grasping the complexities of depression, and how these factors can be influenced through lifestyle changes and targeted interventions
Through my exploration of neurotransmitter imbalance symptoms and the role of BDNF in depression, it’s become clear that a multifaceted approach to treatment – one that considers both biological and environmental factors – is essential for effective management and recovery
By shedding light on the neuroscience behind depression, my goal is to empower individuals with a deeper understanding of their condition, encouraging them to seek evidence-based treatments and to adopt preventative strategies that promote long-term mental well-being
Unveiling the Complexity
Depression is not just a cloud that follows you, it’s a intricate web of neural pathways, stress hormones, and gut health that can be rewoven with the right understanding of neuroscience and a commitment to self-care.
Dr. Anya Sharma
Beyond the Darkness: A Path Forward
As I reflect on the complex interplay between neuroplasticity, gut health, and stress hormones, it becomes clear that unraveling the mysteries of depression requires a multifaceted approach. By exploring the links between neurotransmitter imbalance, BDNF, and treatment options, we can begin to develop a more nuanced understanding of this debilitating condition. My experience as an emergency room doctor has taught me that every individual’s journey with depression is unique, and it’s essential to approach each case with empathy and a commitment to evidence-based treatment.
As we move forward, it’s essential to remember that healing is possible, and that by embracing the latest advancements in neuroscience and treatment options, we can empower individuals to take control of their mental health. By shedding light on the neuroscience of depression, we can work towards a future where this condition is no longer stigmatized, but rather understood and addressed with compassion and cutting-edge care. As someone who’s passionate about debunking medical misinformation, I’m heartened by the progress we’re making, and I’m confident that together, we can create a brighter, more informed future for all.
Frequently Asked Questions
How do stress hormones like cortisol impact the development and progression of depression?
As I’ve seen in my patients, stress hormones like cortisol can wreak havoc on mental health, disrupting the delicate balance of neurotransmitters and contributing to depression’s development and progression, with chronic elevation of cortisol levels potentially altering neural circuits and exacerbating symptoms.
Can lifestyle changes such as diet and exercise actually influence neuroplasticity and improve depressive symptoms?
As a doctor, I’ve seen lifestyle changes make a significant impact on neuroplasticity and depressive symptoms. A balanced diet rich in omega-3 fatty acids and regular exercise, such as my own favorite, long-distance cycling, can boost neurotrophic factors like BDNF, promoting a healthier brain and alleviating depression.
What role does BDNF play in the treatment of depression, and how can it be increased through natural means or medication?
As I’ve seen in my patients, BDNF (Brain-Derived Neurotrophic Factor) plays a crucial role in depression treatment, promoting neural growth and connection. Increasing BDNF can be achieved through natural means like exercise, meditation, and omega-3 rich diets, or medication such as antidepressants, which have been shown to boost BDNF levels.